The patient

Patient right profile
Bilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Ms N.H
First visit : 09/20/2016
Last visit : 01/30/2018
Ms. N.H is a 33-year-old female with no previous medical history or any known keratoconus in her family .
She complained of a progressive decrease in visual acuity greater in the right eye than the left.
The diagnosis of keratoconus was made in 2016 in other institution. At that very first visit, a corneal collagen cross linking (CXL) procedure was proposed. The patient decided not to undergo the cross-linking procedure and came to us for a second opinion.
Her refraction was RE 20/30 with -2.50 (-3.25 x 140°) and LE 20/20 with -1.50 (-1.50 x 150°)
When asked about the possibility of eye rubbing, she admitted to frequently rubbing her eyes with rotating movements of the fists and knuckles since childhood, for the « comfort and pleasurable sensations it induced », and she would repeatedly describe to us « how good it feels when you rub your eyes for 10 to 20 seconds continuously ».
We found bilateral Vogt’s striae and Fleischer rings (Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin) in both eyes.
Corneal topography revealed the presence of bilateral keratoconus more pronounced in the right eye.
As eye rubbing preceded the onset of the corneal deformation by many years, and because eye rubbing in itself is sufficient to induce a permanent corneal warpage (once the corneal native resistance cannot uphold the incident repetitive traumatic forces), we advised the patient to stop rubbing her eyes. She understood our explanation and was motivated to stop rubbing, as she was afraid of losing more of her vision.
At the following visits, she told us that she used to wake up with the irritated right eye and that she used to sleep on the right side. We prescribed an eyeshield protection.
In such cases, vision cannot be restored by spectacle correction. Rigid gas permeable (RGP) or scleral contact lenses would then be required. This patient was fitted with RGP lenses.
Here are pictures of patient rubbing her eyes and her profiles
Here a video of patient showing how she used to rub her eyes
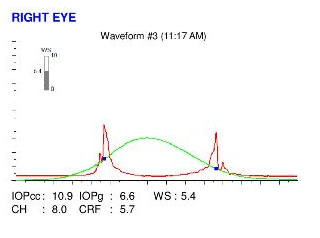
Here are the Orbscan quadmaps, Pentacam maps and Ocular Response Analyzer (ORA) results of the first visit .
Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The keratoconus is stable, more than 16 months after the patient definitively stopped rubbing her eyes.
This patient stopped rubbing her eyes since being sensitized to the deleterious effects of eye rubbing at her first visit. She felt that her eyes were generally more comfortable than when she was actively rubbing her eyes. Eye rubbing can temporarily relieve local irritation, but it increases local inflammation in the long run, because of the induced friction on the ocular surface, and the possible contamination with germs, irritants and allergens.
In this case, bilateral eye rubbing with the fists and knuckles preceded the appearance of keratoconus by many years. Both right and left eyes have keratoconus of similar stage. There was no allergy or history of atopy. The patient simply enjoyed eye rubbing, which she found pleasurable by inducing a sense of calm in her. This case strongly suggests that eye rubbing can trigger keratoconus, even when there are no associated allergies and atopic conjunctivitis. Cross linking is never an urgent procedure, as our wide experience shows that the cessation of eye rubbing is sufficient to stabilize corneas with keratoconus of any stage.
Cross-linking is a technique thought of and conceived to stiffen the cornea (through the collagen of the corneal stroma). However, the stiffening of the cornea has not been observed or documented in clinical conditions (in vivo). Some doctors claim that CXL must work, hence the instruments are failing to measure the stiffening post-operatively (while these instruments would not fail to measure any further weakening, curiously). In our opinion, the lack of stiffening outside of in vitro experimentation means that for reasons that should be explored further, CXL fails to restore impaired corneal biomechanics significantly. In fact, the body of observations we collect everyday teaches us that keratoconus is not a primary inherited corneal collagen disease, but the result of excessive local trauma (eye rubbing). Hence, it is more important to stop the root cause mechanism (eye rubbing) than to try to stiffen a cornea that is focally but not globally weakened, as demonstrated by recent studies.
While some observations suggest that CXL could stabilize some corneas with keratoconus, some meta-analyses have tempered this conclusion (see Cochrane library conclusions about keratoconus and CXL).
While some patients are anxious to get a procedure recently approved by the United States FDA and often presented as a « cure for keratoconus » performed on themselves, some others, like this patient, are skeptical and reluctant to undergo a possibly invasive procedure (the irradiation of the corneal stroma with UV light creates free radicals and keratocytes apoptosis, which may not be desirable on tissues already damaged by the excessive rubbing forces). The progression of keratoconus is slow, over a matter of months, not days. There is therefore never any urgency to perform cross-linking. It is better to temporize and reexamine the patient a few weeks later. Most importantly, proper information about eye rubbing must be given to the patient, and the benefits brought about by the cessation of this habit clearly explained.
In our experience, all patients who stopped rubbing their eyes have shown no progression of their disease. These experiences are shared on this site, and should give hope to the many patients with keratoconus.