Patient right profile
Case #99
The patient

Unilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Mr B.K
First visit : 10/02/2013
Last Visit : 10/23/2018
Mr. B.K is a 19-year-old male prison guard with asthma (atopy) in his medical history and no known family history of keratoconus (he has two brothers who have no history of keratoconus). Keratoconus was diagnosed in July 2018 in another institution. He complained of a progressive decrease in visual acuity greater in the left eye than the right one.
His refraction at the first visit at the Rothschild Foundation (on 02/10th/2018) was : Right Eye (RE) 20/32 with +0.50 (-2.25 x 50 °) and Left Eye (LE) 20/50 with -0.5 (-2.00 x 25 °).
Clinical examination with the slit lamp suggested a thin and irregular left cornea with sub-epithelial opacities and corneal fibrosis, with dry eyes. We also noted an aspect of anterior iris atrophy inferiorly, in the left eye only. This was associated with a depigmentation and disorganization of the anterior leaf of the iris stroma. The natural convexity seemed interrupted, with a slight convexity along the depigmented zone. These changes correspond to what has been described as iridoschisis.
Corneal topography performed at our institution showed the presence of a bilateral keratoconus, more pronounced in the left eye.
At the first visit, when asked about the possibility of frequent eye rubbing, the patient admitted to rubbing his eyes when working in the jail. He told us that the environment of his work is quite dusty, and that his eyes are often red and itchy at work.
He is right handed but he used to rub more often his left eye which irritates him more. The patient sleeps on his left side, with the head buried in the pillow (pillow hugging). He told us that his mother used to get him to bed on his left side from childhood.
We were intrigued by the the inferior iris lesion of the left eye, and suspected that they were induced mechanically by the intense rubbing habit of the patient. We also explained to him that eye rubbing may have caused his cornea to deform irregularly. We thus strongly advised him to stop rubbing his eyes and to change his unhealthy sleeping position.
At the subsequent visits, he admitted to having difficulty refraining from eye rubbing. We then prescribed him an eye shield for his right eye and lubricant eye drops for both eyes, and this has curbed his desire to rub his eyes.
We strongly advised this patient to stop rubbing his eyes and to change his unhealthy sleeping position.
During follow-up, he recalled rub his eyes sometimes heavily, before his teenage years, during childhood, due again « to some allergic episodes ». He also became conscious of rubbing his eyes at work, where the environment was dusty, and he had since stopped after his last visit.
Here are pictures of the patient rubbing his eyes and his profiles
 PATIENT RUBBING HIS EYES WITH HIS KNUCKLES. The patient rubs is left eye more than his right eye. This may be related to his particular sleeping position, where the left eye is buried in the pillow and induces ocular discomfort and irritation upon awakening.
PATIENT RUBBING HIS EYES WITH HIS KNUCKLES. The patient rubs is left eye more than his right eye. This may be related to his particular sleeping position, where the left eye is buried in the pillow and induces ocular discomfort and irritation upon awakening. PATIENT DEMONSTRATING HIS SLEEPING POSITION . (LEFT SIDE). He alludes to consistently adopting this position to fall asleep. A pillow is firmly pressed against the right side of his face
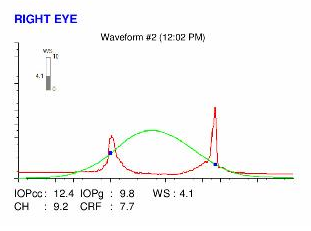
PATIENT DEMONSTRATING HIS SLEEPING POSITION . (LEFT SIDE). He alludes to consistently adopting this position to fall asleep. A pillow is firmly pressed against the right side of his faceHere are the Pentacam maps, Ocular Response Analyzer (ORA) and OCT epithelial maps results of the first visit .
 LEFT EYE ORBSCAN (1st VISIT). Note the increased prolateness (negative asphericity) and toricity (astigmatism) of the anterior (top right) and posterior (top left) corneal surfaces (island pattern). On the curvature map (bottom left), irregular astigmatism is characterized by a marked inferior - central steepening. The thickness map (bottom right) shows central thinning with slight displacement of the thinnest point. The keratoconus is more pronounced in this side.
LEFT EYE ORBSCAN (1st VISIT). Note the increased prolateness (negative asphericity) and toricity (astigmatism) of the anterior (top right) and posterior (top left) corneal surfaces (island pattern). On the curvature map (bottom left), irregular astigmatism is characterized by a marked inferior - central steepening. The thickness map (bottom right) shows central thinning with slight displacement of the thinnest point. The keratoconus is more pronounced in this side.Difference maps have been performed at each subsequent visit. No evolution has been observed between the first and last visit. The keratoconus is still stable, more than 1 month after the patient has definitely stopped to rub his eyes .
In this case, the asymmetry between the deformation in the right and left eyes is striking. We find many instances of ocular friction and compression here, like eye rubbing triggered by dusty environnement and an unhealthy sleeping position.
Another interesting aspect of this case is the patient’s thin corneas. For the same rubbing intensity, a thin cornea may not absorb and dissipate the incident energy as well as a thicker cornea.
About iridoschisis, we explain it by the fact of the proximity of the iris, as the anterior chamber narrows peripherally, would make its anterior part vulnerable to the rubbing effect, causing its depigmentation. The cornea being thicker in its extreme periphery, provides longer resistance to repeated eye rubbing, which would explain the later onset of the disease. A case of bilateral iridoschisis associated with keratoconus has been recently reported in an atopic patient. A conglomeration of these signs and conditions point to a common denominator: incessant and compulsive eye rubbing as the cause.
It is very important to spend time with the patient to elucidate the need for eye rubbing. Often the answers are not apparent at the first consultation, because the patient is not always conscious of the habit. Hence the importance of re-interrogating the patient at each consultation to make him aware of his rubbing habits.
This case is very informative and demonstrative of the direct involvement of eye rubbing and compression in the pathogenesis of keratoconus. Atopy and Environnement is a classic risk factor associated with the disease (as in many cases on this site), but it might just be because allergic patients do rub their itchy eyes way more often and firmly than non allergic patients.
The cessation of eye rubbing and proper allergy therapy along with the correction of the sleeping position are the best tools in the prevention of the genesis and/or evolution of keratoconus.
Other cases :
- Date 23 octobre 2019
- Tags Allergy, Asymmetric, Bilateral keratoconus, Childhood rubbing, Cross-linking like effect, Eczema, Eye rubbing, Iridoschisis, Knuckles rubbing, Male, Palm rubbing, Pillow hugging, Sleep position