The patient

Patient right eye profile
Bilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Mr U.D
First visit : 02/24/2017
Last Visit : 06/26/2018
Mr. U.D is a 17-year-old male with no previous medical history, or any history of keratoconus in the family .
He has known allergy to dust mites, and complains of a progressive decrease in visual acuity in both eyes.
His refraction at the first visit (02/24th/2017) was : Right Eye (RE) 15/20 with -1,5 (-7,75 x 25 °) and Left Eye (LE) 20/20 with -0,5 (-2,75 x 115 °).
Clinical examination with the slit lamp suggested an irregular inferior corneal bulge bilaterally, but more pronounced in the right eye . We also detected discrete bilateral Fleischer rings (Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin), and tarsal papillae (indicating chronic ocular allergy) in both eyes.
Corneal topography revealed the presence of bilateral keratoconus more pronounced in the right eye.
When asked about the possibility of frequent eye rubbing, the patient admitted to rubbing his eyes with his fists and knuckles. His mother, who was present at the consultation, confirmed that she often witnessed her son rubbing his eyes quite vigorously. The eye rubbing commenced some years ago, long before his vision became compromised.
We explained to the patient that since vigorous eye rubbing had preceded the drop in visual acuity, this habit may have caused his cornea to deform progressively. The correlation between the more advanced side (right eye) and the eye rubbed more frequently (right eye) eloquently confirmed this possibility. The preferential position of sleep (the right side) resulting in compression of the right eye may also explain the patient’s tendency to rub this eye more frequently. The latter succumbs to irritation at night when compressed against the pillow, and there is increased contamination with dust mites, etc.
We explained all these factors to the patient, and strongly advised him to stop rubbing his eyes and to change his unhealthy sleeping position.
We treated his allergy aggressively and scheduled him for visual rehabilitation with rigid gas permeable contact lenses.
Here are pictures of the patient rubbing his eyes and his profiles
 PATIENT RIGHT PROFILE
PATIENT RIGHT PROFILE PATIENT LEFT PROFILE
PATIENT LEFT PROFILE PATIENT SHOWING HIS SLEEPING POSITION (ON HIS RIGHT SIDE). This position compresses the right eye and predisposes it to contamination from dust mites and other irritants in the pillows and bed linen.
PATIENT SHOWING HIS SLEEPING POSITION (ON HIS RIGHT SIDE). This position compresses the right eye and predisposes it to contamination from dust mites and other irritants in the pillows and bed linen.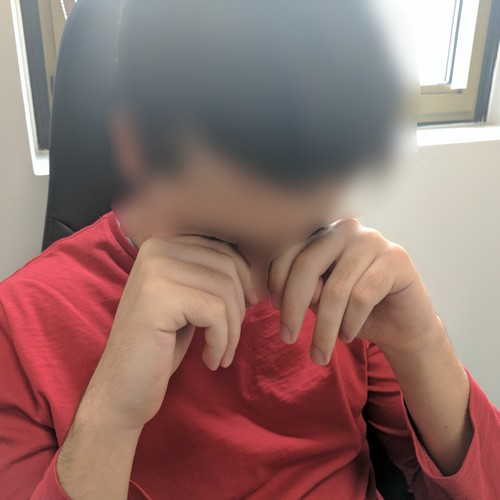 PATIENT RUBBING HIS EYES. Note the typical rubbing fashion often adopted by patients with keratoconus. Patients who rub their eyes with their knuckles (the most rigid part of the hands) are more prone to weakened corneal biomechanics which result in permanent corneal deformation (buckling).
PATIENT RUBBING HIS EYES. Note the typical rubbing fashion often adopted by patients with keratoconus. Patients who rub their eyes with their knuckles (the most rigid part of the hands) are more prone to weakened corneal biomechanics which result in permanent corneal deformation (buckling).Here are the Orbscan maps, OPDscan maps (topography and aberrometry) Pentacam maps, Ocular Response Analyzer (ORA) results and Visante OCT (Optical Coherence Topography) images of the first visit .
 RIGHT EYE ORBSCAN (1st VISIT). There is marked asymmetry on the curvature map (bottom left). Increased prolateness (negative asphericity) and toricity (astigmatism) leads to a marked ridge-island pattern on both anterior (top left) and posterior (top right) corneal elevation maps; The cornea is thinned centrally. This is a typical keratoconus pattern. The cornea is permanently deformed, as if it has been "folded" in the center. This is the result of repetitive trauma, cause by the grinding motions of the knuckles.
RIGHT EYE ORBSCAN (1st VISIT). There is marked asymmetry on the curvature map (bottom left). Increased prolateness (negative asphericity) and toricity (astigmatism) leads to a marked ridge-island pattern on both anterior (top left) and posterior (top right) corneal elevation maps; The cornea is thinned centrally. This is a typical keratoconus pattern. The cornea is permanently deformed, as if it has been "folded" in the center. This is the result of repetitive trauma, cause by the grinding motions of the knuckles.Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The keratoconus is stable, more than 7 months after the patient definitively stopped rubbing his eyes.
This case is very informative and demonstrative of the direct causal effect of eye rubbing in the pathogenesis of keratoconus. Eye rubbing preceded the onset of keratoconus (or at least its progression to a stage where visual impairment is perceptible) by several years. Allergy is a classic risk factor for the disease, as allergic patients tend to rub their itchy eyes way more often and more firmly than non-allergic patients.
In such cases, when the patient is young, the risk of keratoconus progression is statistically higher. Although young patients tend to be less compliant in general to recommendations and medications, if proper and diligent explanations on the benefits of stopping the eye rubbing habit are enforced, the outcome can be truly rewarding. We also encouraged the mother to assist by alerting her son to any unconscious rubbing episodes.
For all our patients, a review visit is scheduled a month after the first visit to monitor keratoconus progression. More importantly, this visit enables us to discuss again with the patient the eye rubbing habit. Usually at this stage, most patients would share with us that they had come to realize how much and how frequently they were rubbing their eyes unconsciously.
In other centers, corneal collagen crosslinking (CXL) is often suggested immediately to patients upon diagnosis of keratoconus. As demonstrated in this case, this practice is unnecessary. In this patient, despite a young age and supposed « aggressive keratoconus », stability of keratoconus was attained simply by the cessation of eye rubbing.
There is never any urgency to perform cross-linking!


























