The patient

Patient right profile
Bilateral Keratoconus induced by eye rubbing
Identity : Ms G.E
First visit : 05/16/2017
Last Visit : 07/25/2017
Ms. G.E is a 23-year-old female student with no previous medical history, or any known keratoconus in her family. She complained of a progressive decrease in visual acuity more pronounced in the right than in the left eye.
Her refraction at the first visit (05/16th/2017) was : Right Eye (RE) 20/25 with -0.25 (-5.25 x 165 °) and Left Eye (LE) 20/60 with +0.25 (-6 x 15 °).
Clinical examination with the slit lamp revealed thin corneas and a suspicion of a slight bilateral paracentral bulging. The corneal nerves were prominent.
Corneal topography revealed the presence of bilateral keratoconus more pronounced in the right eye.
When first questioned about the possibility of frequent eye rubbing, the patient admitted to rubbing her eyes with her fists and knuckles in circular movements. She is right-handed and sleeps preferentially on the right side.
She was born in Guinea where she lived till she was 19 years of age. At the subsequent visits, she verbalised experiencing increased ocular sensitivity in her childhood and teenage years because of the dry, dusty winds in Guinea.
We explained to the patient that since vigorous eye rubbing had preceded the drop in visual acuity, this habit may have caused the cornea to deform in her case. We strongly advised the patient to stop rubbing her eyes. She was then scheduled for a 2nd examination a few months after the initial visit.
Here are pictures of the patient rubbing her eyes and her profiles
 PATIENT RIGHT PROFILE
PATIENT RIGHT PROFILE PATIENT LEFT PROFILE
PATIENT LEFT PROFILE PATIENT SHOWING HER SLEEPING POSITION (RIGHT SIDE). This position compresses the right eye against the pillow and may increase local heating as well as the risk of contamination with irritants and allergens from the linen.
PATIENT SHOWING HER SLEEPING POSITION (RIGHT SIDE). This position compresses the right eye against the pillow and may increase local heating as well as the risk of contamination with irritants and allergens from the linen. PATIENT RUBBING HER EYES. The circular movements with knuckles and fingers are quite vigorous and proceeds for more than a few seconds each time. The patient admits to rubbing her eyes in the mornings upon awakening, and at night before sleeping.
PATIENT RUBBING HER EYES. The circular movements with knuckles and fingers are quite vigorous and proceeds for more than a few seconds each time. The patient admits to rubbing her eyes in the mornings upon awakening, and at night before sleeping.In this video, you can see how Ms F.D rubs her eyes with circular movements of her fingers. These intense and repetitive movements are certainly responsible for the induction of corneal deformation: the force exerted on the corneal wall is considerable in relation to the native biomechanical strength of the cornea.
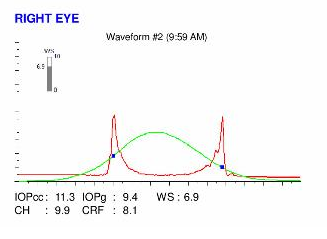
Here are the Orbscan quadmaps, Pentacam maps, OPDscan (topography and aberrometry) maps and Ocular Response Analyzer (ORA) results of the first visit .
Difference maps were performed at the second visit. The patient declared that she had come to realise that she rubbed her eyes more in the past than she was aware of at the first visit. No evolution was observed between the first and second visits. The keratoconus is currently stable, more than 2 months after the patient definitively stopped rubbing her eyes .
In this case, chronic eye rubbing preceded the corneal deformation and subsequent drop in visual acuity. Circular movements caused the corneal to buckle more centrally than when the rubbing is exerted inferiorly. The cessation of eye rubbing resulted in the stabilization of the corneal deformation.
Fortunately, not all patients who rub their eyes develop keratoconus. This is where genetic susceptibility may come into play. It could correspond to the induction of a more « fragile » cornea phenotype ( « softer », « finer ») which is more prompt to deform under the action of mechanical stress (friction) than a stiffer and thicker cornea.
The genetic modulation of immunity leading to allergy could also play a role in keratoconus susceptibility. Allergies result in pruritus and a tendency to rub, and it is thus easy to explain the association between allergy and keratoconus.