The patient

Patient right profile
Bilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Ms T.H
First visit : 01/31/2013
Last Visit : 11/16/2017
Ms. T.H is a 25-year-old female with allergy to dust mites but with no known history of keratoconus in the family. She first consulted us for a refractive surgery suitability assessment. She complained of a progressive decrease in visual acuity in both eyes.
Her refraction at the first visit (01/31th/2013) was : Right Eye (RE) 20/20 with +0.5 (-4.5 x 180 °) and Left Eye (LE) 20/20 with +0.25 (-4 x 5 °).
Clinical examination with the slit lamp revealed an irregular inferior corneal bulge and thin cornea in both eyes.
Systematic corneal topography performed routinely for every refractive surgery candidate revealed bilateral keratoconus, more pronounced in the right eye.
At the first visit, we asked her about possible eye rubbing habits. The patient denied any eye rubbing at first. When asked about her sleeping habits, the patient informed us that she sleeps on her right side with her head in the pillow (« pillow hugging »). She is right-handed.
During subsequent visits, the patient confessed that she had become aware of rubbing her right eye several times a day, especially in the mornings with her right hand, using the knuckles as well as her nails.
We explained to the patient that since vigorous eye rubbing had preceded the drop in visual acuity in her case, this habit may have caused the cornea to deform. We strongly advised her to stop rubbing her eyes, and to change her unhealthy sleep position.
In this case, the asymmetry between the right and left eye deformation is striking. It is correlated with her sleeping posture and eye rubbing habit.
After being sensitised to the deleterious effects of eye rubbing, she subsequently stopped rubbing her eyes.
Topography performed at her last two visits showed strictly stable differential topographic maps. Thus the definitive stoppage of eye rubbing resulted in stability of the disease. We contemplate performing PRK on her corneas which will serve a dual purpose: a refractive correction resulting in a functional improvement of visual acuity and a therapeutic effect of reducing corneal sensation and consequently a reduction in the desire to rub the eye.
Here are pictures of the patient rubbing her eyes and her profiles
 PATIENT RIGHT PROFILE
PATIENT RIGHT PROFILE PATIENT LEFT PROFILE
PATIENT LEFT PROFILE PATIENT SLEEP POSITION (ON THE RIGHT SIDE). The patients shows how she presses the hand and pillow against her face, causing local compression of the orbital area.
PATIENT SLEEP POSITION (ON THE RIGHT SIDE). The patients shows how she presses the hand and pillow against her face, causing local compression of the orbital area. PATIENT RUBBING HER RIGHT EYE. She uses the lateral part of her index finger, in horizontal and circular movements.
PATIENT RUBBING HER RIGHT EYE. She uses the lateral part of her index finger, in horizontal and circular movements.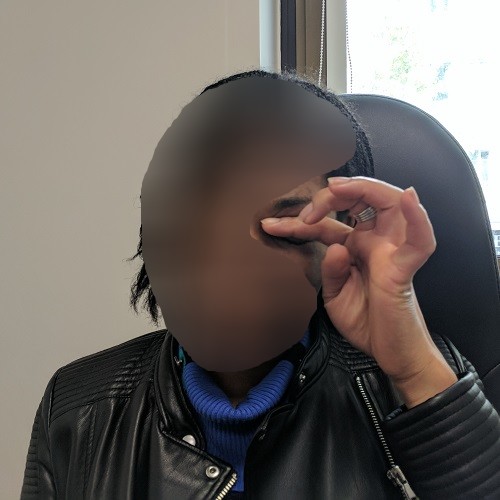 PATIENT RUBBING HER LEFT EYE. She rubs with the lateral side of the index finger, in circular movements.
PATIENT RUBBING HER LEFT EYE. She rubs with the lateral side of the index finger, in circular movements.Here are the Orbscan quadmaps with SCORE ANALYSER values, OPDscan (topography and aberrometry) maps and Ocular Response Analyzer (ORA) results of the first visit .
 RIGHT EYE ORBSCAN (1st VISIT). The topographic pattern suggests the existence of an early form of permanent rubbing-induced warpage, with an increased prolateness (central steepening and peripheral flattening), along with irregularities (asymmetric bow-tie pattern on the axial curvature map, bottom left)
RIGHT EYE ORBSCAN (1st VISIT). The topographic pattern suggests the existence of an early form of permanent rubbing-induced warpage, with an increased prolateness (central steepening and peripheral flattening), along with irregularities (asymmetric bow-tie pattern on the axial curvature map, bottom left)BEFORE THE PRK
Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The keratoconus is stable, more than 4 years after the patient had definitively stopped rubbing her eyes .
 PENTACAM DIFFERENTIAL MAPS : RIGHT EYE. The 3rd column (difference map) shows the absence of change between the two compared examinations.
PENTACAM DIFFERENTIAL MAPS : RIGHT EYE. The 3rd column (difference map) shows the absence of change between the two compared examinations. ORBSCAN PACHYMETRY DIFFERENTIAL MAPS : RIGHT EYE (between 1st and 2nd visits). Here, the absence of progression is demonstrated by the absence of change in the corneal thickness values and patterns.
ORBSCAN PACHYMETRY DIFFERENTIAL MAPS : RIGHT EYE (between 1st and 2nd visits). Here, the absence of progression is demonstrated by the absence of change in the corneal thickness values and patterns. PENTACAM DIFFERENTIAL MAPS : LEFT EYE. Perfect stability is demonstrated here between the two compared examinations.
PENTACAM DIFFERENTIAL MAPS : LEFT EYE. Perfect stability is demonstrated here between the two compared examinations. ORBSCAN PACHYMETRY DIFFERENTIAL MAPS : LEFT EYE (between 1st and 2nd visits). As for the right eye, there is no change in the corneal thickness between the first and second examinations; the corneal deformation is stable.
ORBSCAN PACHYMETRY DIFFERENTIAL MAPS : LEFT EYE (between 1st and 2nd visits). As for the right eye, there is no change in the corneal thickness between the first and second examinations; the corneal deformation is stable.AFTER THE PRK (on the 11/16th/2017)
Control visit with OPD and Orbscans maps will be in one month
In this case, the asymmetry in severity of cornea deformation is most certainly due to the fact that the patient rubs her eye more vigorously on one side (the right eye), and sleeps on her right side.
Patients who regularly rub their eyes with the knuckles or nails rather than the pulp of the fingers are particularly at risk of developing keratoconus. The friction induced by the knuckles are intense and when repetitive, will cause a definite modification of the architecture of the corneal dome, with progressive biomechanical embrittlement, resulting in a loss of the regularity of the corneal curvature.
Similarly, the occurrence of continuous eye compression during sleep, in patients sleeping sideways or on the stomach with the head « buried » in the pillow, is a predisposing factor for keratoconus. This sleeping posture, with prolonged contact of the mattress and/or pillow on the patient’s eye, predisposes to ocular irritation on that side. In patients who sleep by « pressing on their eyes », characteristic topographic patterns are observed, marked by the occurrence of a camber more marked inferiorly but without excessive thinning. These changes serve as a stage for the onset of keratoconus; in most cases, the deformation seen in keratoconus is not caused by ocular compression against the pillow per se but by the friction generated by the constant rubbing of an irritated eye.
On this site, we wish to therefore convey the following message: that keratoconus can not appear or evolve without the action of an external mechanical force, which is conveyed by the hands (fingers, knuckles or nails) of patients who rub their eyes. Based on our experience with dozens of well-documented cases on this website, it appears that ocular friction (or repeated mechanical stress) is not the consequence of keratoconus or a mere risk factor, but most likely THE cause of keratoconus.






























