The patient

Patient sleep position
Bilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Mr I.I
First visit : 11/09/2015
Last Visit : 09/08/2017
Mr. I.I is a 31-year-old male who works as a baker. He has no previous medical history or any known family history of keratoconus. He complained of a progressive bilateral decrease in visual acuity, more pronounced in the left eye than the right.
His refraction at the first visit (11/09th/2015) was : Right Eye (RE) 20/20 with -0.75 (-1.5 x 15 °) and Left Eye (LE) 20/40 with -3.25 (-5.5 x 145 °).
Clinical examination with the slit lamp revealed an increased visibility of the corneal nerves. The corneas were transparent but they appeared thinner in the center. A Fleischer ring was observed in the left eye (Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin).
Corneal topography revealed the presence of bilateral keratoconus more pronounced in the left eye.
When questioned about the possibility of frequent eye rubbing, the patient admitted that he rubs his eyes after contact lens removal, after work and in the mornings. He told us that 2 years prior, he noticed his vision decreasing after he had to work in one of his shops to replace an employee, and was exposed to wheat particles which irritated his eyes. Before that he was a manager and was not exposed to the flour and other ingredients used in the making of bread and pastries. During this period, he used to rub his eyes chronically when tired. The patient is right-handed and sleeps on the left side with the head in the pillow (pillow hugging).
At the subsequent visits, he admitted to being less exposed to particles due to his new job status and he had also changed his sleeping position. He also no longer rubbed his eyes after removal of his contact lenses and in the mornings. To quell his urge to rub, he instilled artificial tears or antihistamine eye drops.
We explained to the patient that since vigorous rubbing had preceded the drop in visual acuity, this habit may have caused the cornea to deform.
We strongly advised this patient to stop eye rubbing and to change his unhealthy sleeping position, since it caused a chronic nocturnal compression of the left orbit and the possible contamination of the left ocular surface.
Here are pictures of the patient rubbing his eyes and his profiles
 PATIENT'S SLEEPING POSITION : Note the contact of the left eye with the pillow.
PATIENT'S SLEEPING POSITION : Note the contact of the left eye with the pillow.  PATIENT RUBBING HIS LEFT EYE. He uses his knuckles with rotational and grinding movements
PATIENT RUBBING HIS LEFT EYE. He uses his knuckles with rotational and grinding movements PATIENT RUBBING HIS EYES WITH KNUCKLES. This kind of chronic rubbing is particularly detrimental biomechanically to the cornea.
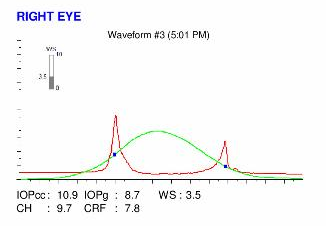
PATIENT RUBBING HIS EYES WITH KNUCKLES. This kind of chronic rubbing is particularly detrimental biomechanically to the cornea.Here are the Orbscans quadmaps, Pentacams, OPDscan (topography and aberrometry) maps and Ocular Response Analyzer (ORA) results of the first visit .
 RIGHT EYE ORBSCAN (1st VISIT). This examination reveals the presence of an asymmetry on the axial curvature map (bottom left), and an increased prolateness on both corneal surfaces (see elevation maps, to left for the anterior and top right for the posterior surface of the cornea). The cornea is thinned centrally.
RIGHT EYE ORBSCAN (1st VISIT). This examination reveals the presence of an asymmetry on the axial curvature map (bottom left), and an increased prolateness on both corneal surfaces (see elevation maps, to left for the anterior and top right for the posterior surface of the cornea). The cornea is thinned centrally.Difference maps have been performed at each subsequent visit. No evolution was observed between the first and last visits. The keratoconus is stable, more than 2 years after the patient had definitively stopped rubbing his eyes .
This case reveals the direct association of occupational exposure to allergenic particles and eye rubbing.
Allergy is a classic risk factor for keratoconus because it is responsible for the induction of significant intense eye rubbing. These repeated frictions have a deleterious mechanical and inflammatory effect on the cornea, often responsible for the thinning and irregular deformation commonly observed.
This patient’s unremarkable background history in his early years contrasts with the late exposure to wheat and dust as an adult , which increased the risk of allergy, resulting in ocular itch triggering eye rubbing. Fortunately, the cessation of eye rubbing resulted in a stabilization of the corneal deformation in his case, without any keratoconus progression.