The patient
 Profile of right eye
Profile of right eyePatient right profile
Bilateral Asymmetric Keratoconus induced by eye rubbing
Identity : Mr C.N
First visit : 04/18/2017
Last Visit : 09/05/2017
Mr. C.N is a 25-year-old male with no previous medical history or known keratoconus in his family. He had been followed up in another institution, and had crosslinking performed in both eyes in 2013. The procedure did not improve his vision, and did not stop the keratoconus from progressing in both eyes. He complained of a progressive decrease in visual acuity greater in the right eye than the left. He did not receive much explanation about his disease from his previous physicians, and thus sought another opinion from us. He could not understand why keratoconus continued to evolve despite crosslinking in his case.
His refraction at the first visit at the Rothschild foundation (on 04/18th/2017) was : Right Eye (RE) 20/200 with -2.75 (-8.25 x 45 °) and Left Eye (LE) 20/60 with -2.5 (-6.75 x 135 °).
Clinical examination with the slit lamp revealed bilateral Vogt’s striae and Fleischer rings. Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin. Vogt’s striae are thin vertical streaks located in the posterior corneal stroma (at the level of the Descemet membrane). These folds disappear with external pressure on the globe.
Corneal topography performed at our institution showed the presence of bilateral keratoconus more pronounced in the right eye.
We investigated the risks factors for eye rubbing at the first visit. This patient disclosed known allergy to dust mites. With regards to his sleeping habit, the patient slept on his right side, with his head buried in the pillow.
When asked about the possibility of frequent eye rubbing, the patient admitted to being aware of rubbing his eyes when he awoke (he often awoke with red eyes), and in the evenings after work. Rubbing gave him a sense of well-being.
At the subsequent visits, he remembered rubbing his eyes sometimes heavily as a child, and especially during periods of allergic episodes.
We explained to the patient that since vigorous rubbing had preceded the drop in visual acuity, this habit may have caused the cornea to deform, leading to the classic clinical presentation of keratoconus. The patient agreed that this pathway was logical and could well explain his keratoconus history. He was concerned about his previous medical follow-ups, as he was only informed that he had a genetic ophthalmic disease, and was never counselled with regards to eye rubbing and keratoconus evolution.
We strongly advised this patient to stop eye rubbing and to change his unhealthy sleeping position.
Here are pictures of patient rubbing his eyes and profiles
 Profile of right eye
Profile of right eye PATIENT RUBBING HIS RIGHT EYE WITH FINGER
PATIENT RUBBING HIS RIGHT EYE WITH FINGER PATIENT SHOWING HIS SLEEP POSITON (ON THE RIGHT SIDE)
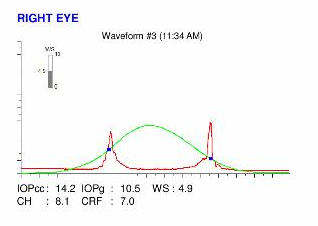
PATIENT SHOWING HIS SLEEP POSITON (ON THE RIGHT SIDE)Here are the Orbscan quadmaps, Pentacam exams, and Ocular Resonse Analyzer (ORA) results of the first visit .
Difference maps were performed at each subsequent visit. No evolution has been observed between the first and last visits. The keratoconus is stable, more than 5 months after the patient had definitively stopped rubbing his eyes .
He began a trail with rigid contact lenses to improve his vision.
In this case, crosslinking was performed, but no significant benefit was observed, as the patient did not receive proper advice on the root cause of keratoconus progression in his case: EYE RUBBING.
On the other hand, crosslinking has not been conclusively proven to be clinically efficient in strengthening the cornea in vivo. No clinical study has ever evidenced any corneal stiffening after CXL in patients with keratoconus. As clearly demonstrated in this case, cessation of eye rubbing is sufficient to arrest the evolution of keratoconus, and surgery (such as crosslinking) is unnecessary. Patient education and making them aware of the importance of the deleterious effects of ocular friction and all other associated factors responsible for ocular friction (sleeping position, allergy, dry eye, prolonged work in front of the computer screen) are the best tools to prevent the occurrence and progression of keratoconus
In our experience, the cessation of eye rubbing is the most important parameter for the control of progression of corneal deformation. In our opinion, keratoconus is not an inherited disease, but the consequence of repeated mechanical trauma. Logically, the cessation of trauma leads to the eradication of the cause of the deformation and thus like many cases on this site, the cessation of eye rubbing arrests the evolution of keratoconus. This website provides many other encouraging examples to support this.