Patient right profile
Case #59
The patient

Bialteral Asymmetric Keratoconus induced by eye rubbing
Identity : Ms C.M
First visit : 05/15/2014
Last Visit : 09/14/2017
Ms. C.M is a 29-year-old female with no previous medical history or any known family history of keratoconus. She complained of a progressive decrease in visual acuity greater in the left eye than the right.
Her refraction at the first visit at the Rothschild foundation (on 05/15th/2014) was : Right Eye (RE) 20/20 with -0.25 (-1.5 x 45 °) and Left Eye (LE) 20/32 with -0.25 (-2.75 x 130 °).
Clinical examination with the slit lamp suggested a thin and irregular left cornea with Fleischer ring. Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin. We also noted bilateral dry eyes with tear film break up time of < 8 secs.
Corneal topography performed at our institution showed the presence of bilateral keratoconus, more pronounced in the left eye
At the first visit, when asked about the possibility of frequent eye rubbing, the patient admitted to rubbing her eyes with her palms and nails, in the mornings, in the shower and after removing eye makeup at the end of the day.
She is left handed and rubs her left eye more often than the right. The patient sleeps on her left side, with the head buried in the pillow (pillow hugging)
We explained to the patient that since vigorous rubbing had preceded the drop in visual acuity, this habit may have caused the cornea to deform, leading to the classic clinical presentation of keratoconus in her case.
We strongly advised her to stop rubbing her eyes and to change her unhealthy sleeping position.
Here are pictures of the patient rubbing her eyes and her profiles
 PATIENT RIGHT PROFILE
PATIENT RIGHT PROFILE PATIENT LEFT PROFILE
PATIENT LEFT PROFILE PATIENT RUBBING HER EYES WITH HER KNUCKLES
PATIENT RUBBING HER EYES WITH HER KNUCKLES PATIENT RUBBING HER EYES WITH HER PALMS. This rubbing gesture is more often seen in women in our experience. The pressure of the palms is directly exerted against the apex of the cornea.
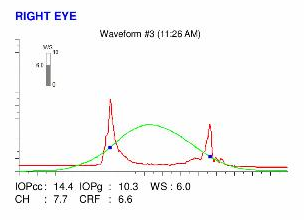
PATIENT RUBBING HER EYES WITH HER PALMS. This rubbing gesture is more often seen in women in our experience. The pressure of the palms is directly exerted against the apex of the cornea.Here are the Orbscan quadmaps with SCORE ANALYZER, Pentacam maps, OPD scans and Ocular Response Analyzer (ORA) results of the first visit .
 RIGHT EYE ORBSCAN (1st VISIT). This map suggests an early corneal warpage, characterized by a hyperprolate asphericity and slight oblique irregular astigmatism. The cornea is markedly thinner in the center, Hyperprolateness corresponds to a marked reduction of the curvature from the steepened center toward the flatter periphery. As the cornea buckles centrally, it flattens peripherally.
RIGHT EYE ORBSCAN (1st VISIT). This map suggests an early corneal warpage, characterized by a hyperprolate asphericity and slight oblique irregular astigmatism. The cornea is markedly thinner in the center, Hyperprolateness corresponds to a marked reduction of the curvature from the steepened center toward the flatter periphery. As the cornea buckles centrally, it flattens peripherally. LEFT EYE ORBSCAN (1st VISIT). This map presents a more pronounced central keratoconus than the right one. The cornea is very thinned in the center, and is markedly hyperprolate (marked reduction of the curvature from the steepened center toward the periphery). Note the increased posterior elevation against the best fit sphere (top right).
LEFT EYE ORBSCAN (1st VISIT). This map presents a more pronounced central keratoconus than the right one. The cornea is very thinned in the center, and is markedly hyperprolate (marked reduction of the curvature from the steepened center toward the periphery). Note the increased posterior elevation against the best fit sphere (top right).Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The keratoconus is stable, more than 36 months after the patient definitively stopped rubbing his eyes .
As shown in this case and others in this website, cessation of eye rubbing is sufficient to prevent the progression of keratoconus, and surgical procedures (such as crosslinking) are unnecessary. Patient education and sensitisation to the deleterious effects of ocular compression and friction, as well as their associated factors and triggers (sleeping position, allergy, dry eye, prolonged work in front of the computer, irritated eyes after a shower) are the best tools to prevent the onset and/or evolution of keratoconus. Women generally rub their eyes less when they wear eye make-up, but many rub their eyes vigorously after eye make up removal, and they must be made aware of this habit.
The corneal dome can be likened to a shell whose equilibrium geometry depends on the difference between the intraocular pressure (exerted on its posterior surface) and the atmospheric pressure. Beyond a certain threshold, the mechanical stresses (compression, shear) conveyed by eye rubbing results in a biomechanical embrittlement, due to the rupture of the harmonious arrangement of collagen fibers, which causes an irreversible deformation of the cornea (This mechanism is analogous to the « buckling » in resistance of materials).
As demonstrated again in this clinical example, the cessation of eye rubbing and patient education are the best tools in the prevention of the genesis and/or evolution of keratoconus.
Autres cas :
- Date 7 décembre 2017
- Tags Asymmetric, Bilateral keratoconus, Central keratoconus, Computer screen, Dry eyes, Enjoyed eye rubbing, Eye rubbing, Female, Knuckles rubbing, Morning rubbing, Nails rubbing, Palm rubbing, Post shower rubbing, Removing makeup rubbing, Sleep position, Work rubbing