Patient right profile
Case #69
The patient

Unilateral Asymmetric Corneal Ectasia post PRK with cross-linking induced by eye rubbing
Identity : Mr B.T
First visit : 04/24/2015
Last Visit : 01/16/2018
Mr. B.T is a 28-year-old male with no previous medical history or any known family history of keratoconus. The patient had bilateral Photorefractive Keratectomy (PRK) combined with corneal collagen cross-linking (CXL) in 2015 performed in another country. Pre-operatively, he had myopia of about -4 D in the left eye and -3D in the right eye. He complained of a progressive decrease in visual acuity greater in the left eye than the right, and monocular diplopia in left eye, 2 years after the procedure. He then consulted us for a second opinion.
His refraction at the first visit at the Rothschild Foundation (on 04/25th/2015) was: Right Eye (RE) 20/20 with+0.25 (-0.5 x 170 °) and Left Eye (LE) 20/60 with +0.5 (-0.5 x 125 °).
Clinical examination with the slit lamp revealed thin corneas and suggested the presence of a slight irregular inferior corneal bulge in the left eye. The rest of the ocular examination was normal.
Corneal topography performed at our institution showed the presence of a unilateral corneal ectasia in the left eye.
At the first visit, when asked about the possibility of frequent eye rubbing, the patient admitted to rubbing his eyes when he awoke in the mornings or at work where he was often exposed to dust. Rubbing his eyes gave him a sense of relief, because his eyes were constantly irritated by the dust.
The patient told us that in the immediate course after the PRK and CXL surgery, his eyes were less itchy, but after 3 months he began to rub his eyes vigorously again. He is right handed but rubbed his left eye with his left hand, because his right hand would often be on the computer mouse and keyboard at work.
When asked about his sleeping position, the patient informed us that he used to sleep on his left side, with the head buried in the pillow (pillow hugging).
His sister apparently had refractive surgery in the same institution (although the exact procedure performed on her is unknown). To date, she has not had any symptoms evocative of ectasia, and the patient acknowledged that she did not rub her eyes as much as he did.
We strongly counselled and encouraged the patient to stop rubbing his eyes and to change his unhealthy sleeping position. We also prescribed him an eye shield to be used on the left eye during sleep. We gave this patient an appointment for a review visit, which was scheduled several months later.
Here are pictures of the patient rubbing his eyes and his profiles
 PATIENT RIGHT PROFILE. The central flattening induced by the PRK sugery is difficult to perceive at this scale.
PATIENT RIGHT PROFILE. The central flattening induced by the PRK sugery is difficult to perceive at this scale. PATIENT LEFT PROFILE. The rapid change of curvature between the central and inferior area of the cornea is perceptible in this profile.
PATIENT LEFT PROFILE. The rapid change of curvature between the central and inferior area of the cornea is perceptible in this profile. PATIENT RUBBING HIS EYES WITH HIS KNUCKLES. This maneuver is particularly detrimental to the corneal structure, as the pressure exerted against the eyes by the most rigid portion of the fingers can be quite strong.
PATIENT RUBBING HIS EYES WITH HIS KNUCKLES. This maneuver is particularly detrimental to the corneal structure, as the pressure exerted against the eyes by the most rigid portion of the fingers can be quite strong. PATIENT DEMONSTRATING HIS SLEEPING POSITION (LEFT SIDE). At night, he presses a pillow against the left side of his face with his left hand.
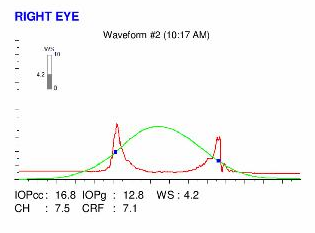
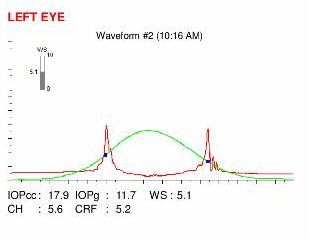
PATIENT DEMONSTRATING HIS SLEEPING POSITION (LEFT SIDE). At night, he presses a pillow against the left side of his face with his left hand.Here are the Orbscan quadmaps, OPD scans, Ocular Response Analyzer (ORA) and OQAS results of the first visit.
Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The corneal ectasia is stable, more than 33 months after the patient definitively stopped rubbing his eyes .
Corneal ectasia post-refractive surgery is a rare but potentially severe complication. It corresponds to a biomechanical decompensation of the cornea, which loses its regularity and whose central curvature increases. Consequently, ectasia results in the reappearance of evolutionary myopia and astigmatism. Corneal ectasia post-PRK is rarer than post-LASIK ectasia. There are several risk factors for ectasia. The main risk factor is the presence of an undetected form of sub-clinical keratoconus existing in the unoperated cornea. As with keratoconus, the habit of repeated eye rubbing is also a risk factor, as these frictions have led to the reduction of corneal resistance before surgery, and the cornea is weakened further if rubbing is continued after the surgery.
This case highlights the risks of eye rubbing after myopic PRK even when combined with corneal cross-linking. Following refractive surgery (LASIK more than PRK), patients often have dry eye, and this gives them a sensation of visual fatigue which is relieved by eye rubbing, which explains why it is not uncommon for patients to describe an intense desire to rub their eyes after corneal refractive surgery.
This case illustrates several other interesting points. Firstly, an indirect benefit of CXL is to induce a reduction in the corneal sensitivity which in turn diminishes pruritus and the desire to rub the eye. The patient describes how his eyes were less itchy immediately and up to 3 months following the PRK and CXL procedure, after which he re-commenced his eye rubbing habits. Secondly and more importantly, corneal collagen cross-linking does not always prevent the development of corneal ectasia when combined with PRK. We do not have in our possession the preoperative topographies, but it is likely to be suspicious or abnormal to warrant a decision by the attending surgeon to perform a surface ablation procedure combined with CXL. This suspicious preoperative topography could well be the result of incessant eye rubbing which has been in existence years before the surgery. This case also tells us that CXL may not be efficacious in patients who continue to rub their eyes. The cessation of eye rubbing succeeded in halting the progression of ectasia, whereas CXL failed to do so.
We can therefore conclude that the main element in ensuring the stabilization of corneal deformation is the cessation of eye rubbing, and this has to be emphasized to all patients with ectasia or keratoconus, with or without cross-linking.
Other cases :
- Date 17 janvier 2018
- Tags Asymmetric, Cross linking, Dry eyes, Ectasia, Enjoyed eye rubbing, Eye rubbing, Knuckles rubbing, Male, PRK, Sleep position