Patient right profile
Case #63
The patient

Bilateral Asymmetric Pellucid Marginal Degeneration stabilized after cessation of eye rubbing
Identity : Mr F.Q
First visit : 06/23/2017
Last Visit : 04/09/2018
Mr. F.Q is a 42-year-old male with no known family history of keratoconus or pellucid marginal degeneration (PMD). He has sleep apnea and a history of myocardial infarction. He complained of a progressive decrease in visual acuity greater in the right eye than the left, which started more than a year prior to presentation. The patient does not have any known allergies.
His refraction at the first visit at the Rothschild Foundation (on 06/23th/2017) was : Right Eye (RE) 20/32 with +5.25 (-7.5 x 75 °) and Left Eye (LE) 20/20 with +0.75 (-1.25 x 80 °).
Clinical examination with the slit lamp suggested a remarkable inferior corneal distortion, with thinning in the inferior cornea from 4 to 8 o’clock.. We also noted an aspect of bilateral anterior iris atrophy inferiorly, more pronounced in the right eye. This was associated with a depigmentation and disorganization of the anterior leaf of the iris stroma. The natural convexity seemed interrupted, with a slight convexity along the depigmented zone. These changes correspond to what has been described as iridoschisis.
Corneal topography performed at our institution showed the presence of a pattern evocative of bilateral Pellucid Marginal Degeneration (PMD), more pronounced in the right eye.
At the first visit, when asked about the possibility of frequent eye rubbing, the patient admitted to enjoying rubbing his eyes when he awoke in the mornings. He also complained of frequent bilateral red eyes upon awakening.
He is right handed and rubs his right eye with his right hand using the knuckles. The patient sleeps on his right side, with the head buried in the pillow (pillow hugging). He acknowledges that he rubs his left eye not as often, as this eye does not feel as irritated as the right eye.
We were intrigued by the bilateral inferior iris lesions, and suspected that they were induced mechanically by the intense rubbing habit of the patient. We also explained to him that eye rubbing may have caused his cornea to deform irregularly. We thus strongly advised him to stop rubbing his eyes and to change his unhealthy sleeping position.
At the subsequent visits, he admitted to having difficulty refraining from eye rubbing. We then prescribed him an eye shield for his right eye and lubricant eye drops for both eyes, and this has curbed his desire to rub his eyes.
Here are pictures of the patient rubbing his eyes and his profiles
 TOP LEFT: Bell's phenomenum refers to an upward and outward movement of the eye, when an attempt is made to close the eyes. In this photo, the patient was asked to close his eyes, and the observer pried the eyelids of the right eye open to demonstrate the Bell's phenomenon. This upward movement of the eye is present in the majority of the population, but its intensity and direction may be variable.
BOTTOM: The bilateral partial iris atrophy (iridoschisis) is visible in the picture as a grayish area inferiorly.
TOP LEFT: Bell's phenomenum refers to an upward and outward movement of the eye, when an attempt is made to close the eyes. In this photo, the patient was asked to close his eyes, and the observer pried the eyelids of the right eye open to demonstrate the Bell's phenomenon. This upward movement of the eye is present in the majority of the population, but its intensity and direction may be variable.
BOTTOM: The bilateral partial iris atrophy (iridoschisis) is visible in the picture as a grayish area inferiorly. Patient showing how he rubs his right eye
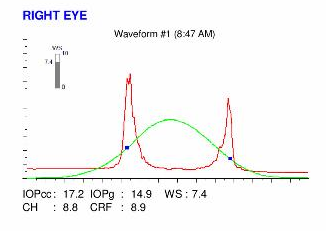
Here are the Orbscan quadmaps, Pentacam maps, OPD scans, Ocular Response Analyzer (ORA) and OCT VISANTE results of the first visit .
 RIGHT EYE ORBSCAN (1st VISIT). This is a typical topography evocative of Pellucid Marginal Degeneration (PMD), with the "crab claw" appearance on the axial curvature map. Also note the reduced axial power along the central vertical axis, and by coupling effect, the increased power along the infero-oblique meridians. There is marked inferior corneal thinning (bottom right). The anterior and posterior elevation maps have a similar pattern, with a very decentered highland pattern.
RIGHT EYE ORBSCAN (1st VISIT). This is a typical topography evocative of Pellucid Marginal Degeneration (PMD), with the "crab claw" appearance on the axial curvature map. Also note the reduced axial power along the central vertical axis, and by coupling effect, the increased power along the infero-oblique meridians. There is marked inferior corneal thinning (bottom right). The anterior and posterior elevation maps have a similar pattern, with a very decentered highland pattern. LEFT EYE ORBSCAN (1st VISIT). This examination shows a mild corneal distortion. The anterior and posterior elevation maps (top) show an increased elevation against the best fit sphere. Slight thinning is perceptible in the paracentral inferior corneal area. This aspect is compatible with an early PMD manifestation.
LEFT EYE ORBSCAN (1st VISIT). This examination shows a mild corneal distortion. The anterior and posterior elevation maps (top) show an increased elevation against the best fit sphere. Slight thinning is perceptible in the paracentral inferior corneal area. This aspect is compatible with an early PMD manifestation. RIGHT EYE PENTACAM (1st VISIT). This examination, performed with a rotative Scheimpflug camera enables us to analyze the corneal curvature (bottom left), the corneal pachymetry (botton center) and the posterior surface elevation against a best fit sphere (bottom right). The vertical field of view is larger than with the Orbscan map. The inferior steepening at the extremity of the inferior meridians is perceptible.
RIGHT EYE PENTACAM (1st VISIT). This examination, performed with a rotative Scheimpflug camera enables us to analyze the corneal curvature (bottom left), the corneal pachymetry (botton center) and the posterior surface elevation against a best fit sphere (bottom right). The vertical field of view is larger than with the Orbscan map. The inferior steepening at the extremity of the inferior meridians is perceptible. LEFT EYE PENTACAM (1st VISIT). This examination shows irregularity in the axial curvature map (bottom left). Interestingly, there is a slight inferior thinning extension on the thickness map (bottom middle). The posterior elevation map shows a zone of higher elevation against the best fit sphere located inferiorly, adjacent to the area of inferior thinning.
LEFT EYE PENTACAM (1st VISIT). This examination shows irregularity in the axial curvature map (bottom left). Interestingly, there is a slight inferior thinning extension on the thickness map (bottom middle). The posterior elevation map shows a zone of higher elevation against the best fit sphere located inferiorly, adjacent to the area of inferior thinning. RIGHT EYE OPDscan topography and aberrometry map. Note the vertical asymmetry (the local keratometries of the upper hemicornea are much lower than those of the lower hemicornea), which generates significant higher order aberrations. Coma and trefoil-like higher aberrations are particularly increased.
RIGHT EYE OPDscan topography and aberrometry map. Note the vertical asymmetry (the local keratometries of the upper hemicornea are much lower than those of the lower hemicornea), which generates significant higher order aberrations. Coma and trefoil-like higher aberrations are particularly increased.Difference maps were performed at each subsequent visit. No evolution was observed between the first and last visits. The Pellucid Marginal Degeneration (PMD) is stable, more than 5 months after the patient had definitively stopped rubbing his eyes .
Classically, pellucid marginal degeneration (PMD) is considered in textbooks and articles as « an ectatic disorder of the cornea which is almost always bilateral, with the deformation in either eye achieved fairly symmetrically. It is typically characterized by a clear, bilateral thinning (ectasia) in the inferior and peripheral region of the cornea« .
This classic description is accompanied by « an arch located in the inferior part of the cornea which protrudes forward, over a peripheral area of corneal thinning« . The « crab claw » pattern on axial curvature maps is a classic feature of corneas with PMD. However, it is not specific, as many keratoconic eyes may disclose a similar pattern.
The term Pellucid Marginal Degeneration was coined for the first time in 1957 in an article written in French by Schlaeppi (« La dystrophie marginale inférieure pellucide de la cornée. » Bibl Ophthalmol. 1957;12(47):672-7). This original paper is not available online, but it is probable that the definition given at that time was not specific and corresponded to some particular visual condition including high against the rule astigmatism caused by a corneal degenerative process incurring a marked inferior (« marginal ») corneal thinning and a preservation of the corneal transparency (« pellucide » means « transparent »). Indeed, the cornea remains transparent as there is neither neovascularisation nor corneal deposits in the course of PMD. The latter is thus differentiated from peripheral corneal disorders associated with inflammation such as Terrien’s peripheral corneal degeneration, Mooren’s ulcer, and ulcers from connective tissue disease.
The advent of computerized corneal specular topography, 3 decades after the first description of PMD, has enabled clinicians to associate the presence of a « crab claw » pattern to situations where a clear extreme inferior paralimbal corneal thinning was present at slit lamp examination. Then, the development of full thickness corneal tomographs (Orbscan, Pentacam) made it possible to objectivate and identify the inferior corneal thinning.
Despite these advances, no specific proximity to the inferior limbus nor distance from the corneal center has been defined. It is interesting to note that the distinction between PMD and keratoconus can be somewhat arbitrary, and based on « fuzzy » criteria. Usually, the presence of band-shaped peripheral corneal thinning, detected by slit-lamp biomicroscopy and confirmed by a pachymetric map, is set as the diagnostic criterion of PMD, to distinguish it from keratoconus. At least, it does seem a fully adopted fact that peripheral and inferior thinning is the hallmark of the PMD, rather than the presence of a claw pattern on axial topography.
The etiology of PMD is unknown, and until now, there have not been any salient pathophysiological hypotheses to account for this corneal disease. Rather, it has been debated that PMD could be a special clinical (inferior) form of keratoconus, based on findings in topography and / or clinicopathologic studies.
The age of onset of PMD is usually later (mean age was found to be 37 in a large survey). While PMD has been classically defined as bilateral, this largest survey to date has documented a relatively high prevalence of unilateral involvement (25%), along with male predominance and the association with allergic diseases.
As we have pointed here, we do not fully agree with the terms of « protrusion » and « ectasia » to describe the shape of keratoconic corneas. Our criticism is supported by this case of a striking example of a typical pellucid marginal degeneration corneal contour. Instead of being « protruded », the corneal wall seems to sag vertically, above a much lower « break zone« . This aspect seems to result from the curvature redistribution after the occurrence of a very inferior corneal buckling, adjacent to the thinned zone.
This observation encourages us to revisit the hypothesis that Pellucid Marginal Degeneration (PMD) is a special form of keratoconus warpage, where the weakened zone of the cornea is so inferior that it causes the corneal curvature to adopt the characteristic claw pattern.
Several elements present in this case support this hypothesis. The pronounced Bell’s phenomenon may predominantly expose the inferior para-limbal corneal area to the impact of knuckle-rubbing. The proximity of the iris, as the anterior chamber narrows peripherally, would make its anterior part vulnerable to the rubbing effect, causing its depigmentation. The cornea being thicker in its extreme periphery, provides longer resistance to repeated eye rubbing, which would explain the later onset of the disease.

The spatial juxtaposition of the zone of thinning and iris depigmentation akin to iridoschisis strongly suggests that these alterations result from the same mechanism. As a consequence of the eye from the strong Bell’s phenomenon, the inferior cornea, limbus, and iris receive the maximum impact of mechanical energy inflicted by eye rubbing.
The similarity in the topographic patterns and clinical history in eyes with PMD and keratoconus suggests that they may be a continuity of the same disorder with different phenotypes and one common feature: excessive eye rubbing. When exerted against the very inferior part of the cornea (adjacent to the limbus), the local thinning and trauma inflicted by eye rubbing causes a marked inferior corneal buckling, which in turns creates a deformation which corresponds to the classic feature of PMD (crab claw pattern). Eye rubbing has been already associated with PMD in one case report. Interestingly, a case of bilateral iridoschisis associated with keratoconus has been recently reported in an atopic patient. A conglomeration of these signs and conditions point to a common denominator: incessant and compulsive eye rubbing as the cause.
The mechanisms by which excessive eye rubbing causes the cornea to thin and deform are detailed here.
In this very interesting case, the cessation of eye-rubbing, together with the protection of the right eye at bed time with an eye shield has stopped the evolution of the pellucid marginal degeneration (PMD). Patient education appears to be the best tool in the prevention of the genesis and evolution of pellucid marginal degeneration .
Autres cas :
- Date 10 décembre 2017
- Tags Asymmetric, Enjoyed eye rubbing, Eye rubbing, Knuckles rubbing, Male, Morning rubbing, Pellucid Marginal Degeneration (PMD), Pillow hugging, Sleep position